If denials, resubmits, and EVV mismatches are eating your week, you’re not alone.
Across Personal Care Services (PCS) agencies, the same pattern keeps showing up: data looks fine in EVV, but payer-specific edits aren’t enforced before submit—so claims bounce back, cash flow wobbles, and staff re-key the same work.
Carehandler was built to break that loop with a simple, reliable path:
EVV → clean claims → faster reimbursement.
Agencies running our workflow report 97% EVV compliance and 99% first-pass claim approval, which translates to fewer touchbacks, fewer surprises, and calmer payroll weeks.
Why denials happen (even when EVV “looks good”)
Most avoidable denials trace back to gaps between EVV data and payer rules:
Service codes/modifiers don’t match plan rules
Missing authorizations or unit alignment
Unscheduled visits or incomplete validations
Overlapping/duplicate visits
Timestamp windows outside billable ranges
When these are caught after submission, your team eats the delay and the rework. When they’re caught before submission, denials drop—fast.
The Carehandler path: EVV → Clean Claims → Faster Reimbursement
Carehandler enforces the edits that matter before a claim leaves the house:

Sandata-friendly, Medicaid Ready PCS workflow
Configurable payer edit rules aligned to your EVV data
Clean-claim checkpoints you can see and control
Audit trails and denial-prep reports when attention is needed
Outcome: Agencies report 99% first-pass claim approval and fewer resubmits, which shows up as steadier DSO and hours back for your billing team.
Proof in practice
Most recent checks our agencies have received Medium to small agencies.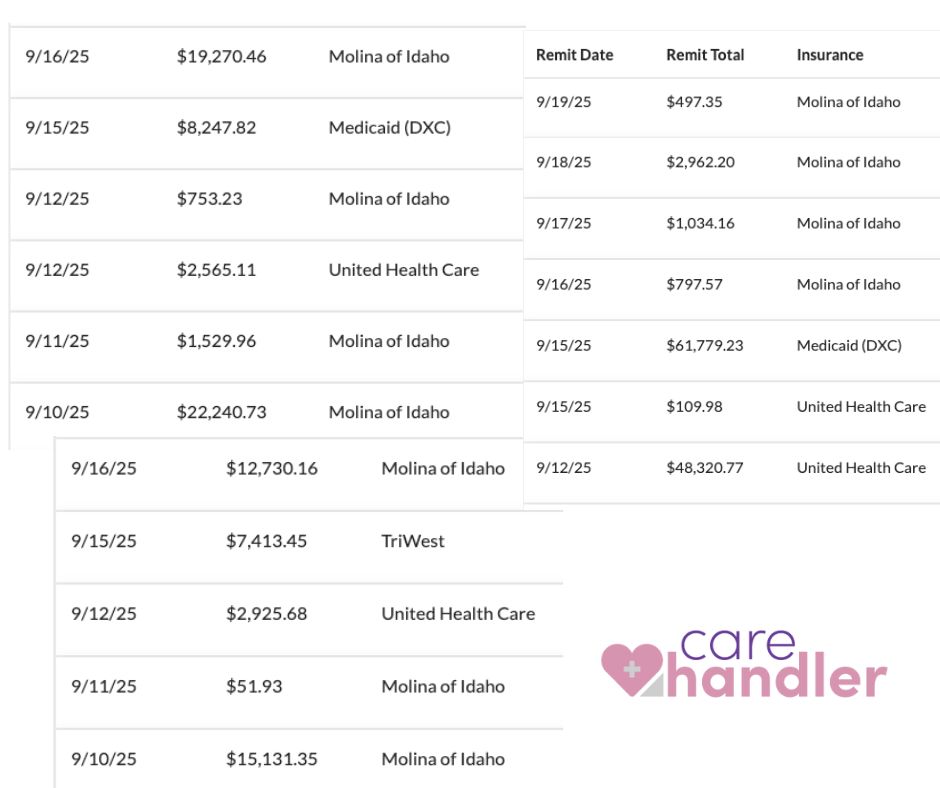 Note: Results vary by payer mix and existing processes. We focus on operational outcomes (denials, first-pass %, hours saved) without requesting PHI by email.
Note: Results vary by payer mix and existing processes. We focus on operational outcomes (denials, first-pass %, hours saved) without requesting PHI by email.
Quick pre-submit checklist (steal this)
Seven checks PCS teams use to cut avoidable denials:
Auth/units aligned to payer rules
Service codes + modifiers match the care plan
Unscheduled/missing validations flagged
Caregiver eligibility/licensure on file
EVV timestamps within billable windows
Duplicate/overlapping visits prevented
Payer-specific edits applied before submission
Carehandler automates these checks so clean claims go out the first time.
What you’ll see in a 30-minute walk-through
The EVV checkpoints that matter for clean claims
How payer edit rules are configured and enforced
Where audit trails explain exactly why a claim is clean
How we stay Sandata-friendly and Medicaid Complaint
FAQ (quick hits)
Do we need to change payers or clearinghouses?
No. Carehandler is Sandata-friendly and Medicaid Compliant, and we fit your PCS workflow.
Will you need PHI for the demo?
No. We can demonstrate with de-identified or sample data.
How fast can we see impact?
Most teams start with a few high-impact edit checks; you can see results as early as the first billing cycle.
What about audits and denials that still occur?
You’ll have audit trails and denial-prep reports so your team knows what changed and why.
Bottom line
PCS billing shouldn’t feel like guesswork. When EVV and payer edits line up before submit, denials drop, first-pass rates climb, and cash flow steadies. If that sounds good, let’s walk through it together.
Book a 30-minute walk-through → Sign Me Up
